Quick Links
For Patients
For Physicians
- Refer a patient to a specialist
- Order labs for patients
- Order radiology for patients
- Order At-Home Services
- Get your practice listed
For Companies
© Copyright 2024 American TelePhysicians. All rights reserved.





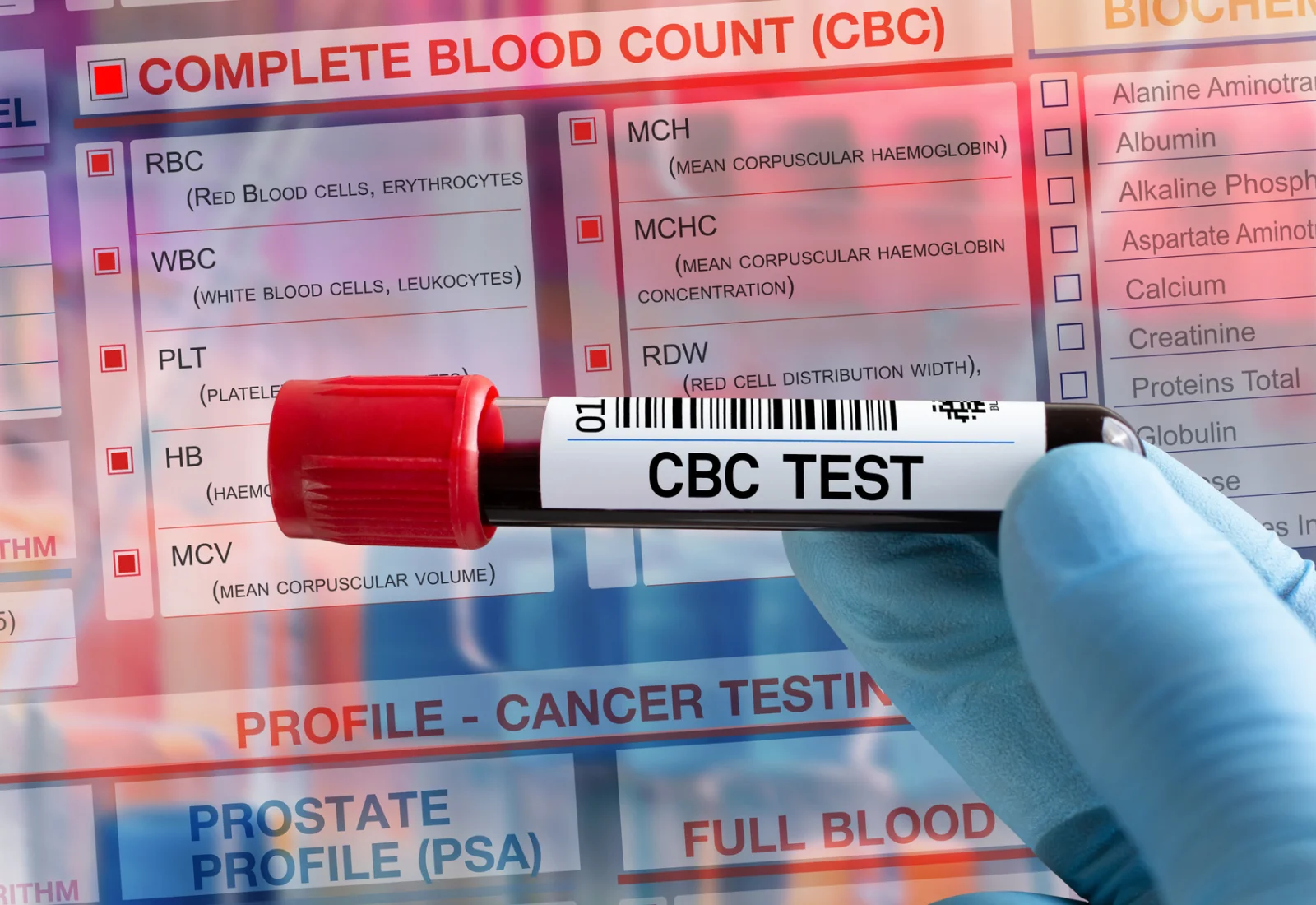
Acute Myeloid Leukemia (AML) is a kind of acute leukemia (cancers of blood cells) that affects a group of white blood cells called myeloid cells, which develop into several mature blood cells such as red blood cells, white blood cells, and platelets. "Acute" means that if the leukemia isn't treated, it will likely worsen quickly. AML causes abnormal myeloblasts (a kind of white blood cell), red blood cells, or platelets to form in the bone marrow. When abnormal cells crowd out healthy cells, infection, anemia, and frequent bleeding can occur. The abnormal cells can also move to other body sections outside the bloodstream.
AML can be divided into various subtypes. The subtypes are determined by how far the cancer cells have progressed and how different they are from normal cells at the time of diagnosis.